Musculoskeletal Conditions
Head/Neck/Jaw
Cervical Radiculopathy
Exercise is effective in promoting analgesia in a variety of chronic musculoskeletal conditions. This is achieved via the ability to activate conditioned pain modulation descending inhibitory pathways which results in subsequent pain relief. Studies have supported that the improvement of cervical function can be achieved by restoring the normal muscle balance through strengthening muscles and stretching tight muscles. Strengthening exercises aim to improve resting neck posture, reduce pain, and may decompress neural elements. A program tailored to the individual can address these main rehabilitation goals and reduce and manage pain in cervical radiculopathy.
Whiplash
Vertigo
Vertigo occurs due to imbalances within your inner ear (the vestibular labyrinth – the part of your ear responsible for balance), a mismatch between the information coming from your inner ear compared to your vision, as a reaction to certain drugs, can be stress related, or even occasionally from your cervical spine (neck) or brain.
There are many potential causes but the most common are infections or diseases in the inner ear such as vestibular neuritis, labrynthitis, Meniere’s disease and Benign Paroxysmal Positional Vertigo (BPPV). Migraines are other common causes.
Symptoms of Vertigo include:
- Feeling of head spinning, rocking or moving
- Feeling of the world spinning, rocking or moving around you (motion sickness)
- Nausea and vomiting
- Looking pale
- Sweating
- Abnormal, uncontrollable, jerky eye movements (nystagmus)
- Ringing or abnormal noises in your ears (tinnitus) or ear fullness
- Balance issues
- Headaches
Symptoms can be acute or have a delayed onset, ranging from mild, long-lasting symptoms to sudden, severe symptoms and avoidance of function. Depending on the condition it can last a few days to months and even years if not managed correctly.
Vertigo Treatment
Vertigo treatment depends on the cause of your symptoms. However, the overarching management approach for all causes are rehabilitation exercises. These are designed to reduce the impact of the symptoms and regain your independence and control over your life. They consist of performing movements or tasks that bring on your symptoms which help to retrain your brain to ignore the incorrect messages coming from you eyes and/or inner ear.
Depending on the cause, medication may help too.
Temporomandibular joint dysfunction / pain (TMD / TMJ)
TMD often occurs alongside other issues such as neck pain and headaches.
TMD can be caused by a wide rage of issues, acting alone or together to cause your symptoms. These include the presence of neck pain and headaches, clenching of your jaw, grinding of your jaw, bruxism (night time clenching and grinding whilst sleeping), increased stress, arthritis, dental issues / recent dental procedures and direct trauma to the face and jaw.
TMD can be rather debilitating, affecting normal, daily tasks such as talking, eating, laughing and sleeping.
Symptoms of TMD include:
- Pain or tenderness about your jaw, mouth, face and / or ear
- Pain and or difficulty with chewing, laughing, talking or smiling
- Stiffness or locking with jaw movements, making it difficult to open and close oyur mouth
- A painful click with jaw movements
- An uncomfortable or uneven bite
TMD Treatment
Practical treatment of TMD involves manual therapy and exercise prescription to relieve the pain and improve function. Recent research has shown that a combination of the above along with a night time guard from a dentist tends to alleviate most issues. Other helpful tips are to avoid hard foods or ones that require significant amounts of chewing. Relaxation techniques and other forms of stress management may further assist. With the above management plan, you should noticeable improvements in your TMD within 1-2 weeks. However, it is worth noting that everyone is different and this is a guide only.
A last resort is surgery but this should not be considered until the above management has been utilised first and has been ineffective.
Neck Pain
Other common causes of neck pain include nerve compression, arthritis causing a stiff neck, whiplash and wry neck. Whiplash is a form of neck pain that occurs typically after a motor vehicle accident where the sudden stop causes a whipping motion to your neck. Fractures can also occur.
Symptoms may vary depending on the cause of your neck pain. These include:
- Pain and/or pins and needles/numbness/tingling in your neck, down your arm and shoulder blade
- Pain and/or difficulty with rotating your head, looking up and/or down
- Tenderness to touch about the neck muscles
- Neck stiffness
- Headaches
Occasionally you can also have dizziness, light-headedness, nausea, blurred vision, and jaw pain.
Neck Pain Treatment
Neck Pain treatment depends upon the issue causing the pain. Acute neck pain often gets better within a few days to 4-6 weeks. If nerve compression occurs then this can take up to 12+ weeks to get better.
General treatment involves being screened for any fractures or emergencies, followed by pain relief and exercises. Pain relief is achieved via manual therapy from a physiotherapist, pain medication and early gentle mobility/strength exercises. As your symptoms subside and function improves, a progressive exercise program will get you back to your previous levels of health and function.
Unless an emergency, surgery should be avoided in the first instance as the vast majority of neck pain can get better with the above approach. Surgery and injections may be of benefit with time if the above approach is proven to be ineffective beyond 12 weeks of pain and loss of function.
To discuss musculoskeletal injuries or treatment in more detail, book a consult and discuss treatment options by booking below or filling out the “We’ll call you” section.
Shoulder
Non-traumatic Shoulder Pain
Shoulder pain is characterised as an overuse (or underuse) injury rather than an impact condition. It generally develops due to either repetitive motions overhead or in extreme ranges of motion. It also usually develops due to a sudden increase in workload on the shoulder. In this case it is either due to a sudden increase in use after a time of inactivity or when you have suddenly upped the ante with your exercise routine even when physically active.
Symptoms of shoulder pain include:
- Pain and or discomfort about the outside, back or front of the shoulder
- Pain and or discomfort with movement overhead or reaching
- Pain with single arm use
Symptoms can be acute or have a delayed onset, ranging from mild discomfort to severe pain and avoidance of function if not treated correctly. It is normal for shoulder pain to last for at least a few months from the time of injury.
Non-traumatic Shoulder Pain Treatment
Practical treatments of shoulder pain include range of motion and strengthening programs for the shoulder and upper body. Current research indicates that progressive, incremental strengthening regimes are an effective treatment tool for increasing pain free function.
Individuals who engage in active rehabilitation early are often able to return to function within 6 weeks. Manual therapy has also shown to assist with pain relief to help you return to the painful tasks early on.
Furthermore, research shows that injections and surgeries should be avoided for at least 6 weeks but ideally not until the above has been trialled over a 3 month time period. Only then should injections and surgery be considered if symptoms and function don’t improve.
Shoulder Subluxation and Dislocation
The most frequent complication with shoulder subluxation and dislocation is recurrence due to instability. Rehabilitation is important to restore dynamic musculature, proprioceptive restraints from shoulder instability and strengthen the rotator cuff muscles supporting the glenohumeral joint. A three-phase approach is typically recommended for shoulder injuries such as dislocations and subluxations. The main goals are to restore pain free range of motion and create stability in the joint before strengthening the supporting rotator cuff muscles and surrounding stabilising muscles.
Rotator Cuff pathology
Some RC tears can be asymptomatic while others can cause debilitating negative symptoms such as pain, loss of strength and function. It is important to note that asymptomatic injuries may or may not progress to being symptomatic and it is unknown why some tears are asymptomatic to begin with.
So, what treatments are available?
The most invasive treatment is surgery, various surgeries exist to reattach, replace, or reconstruct the RC tendons. Surgery is often used along side more conservative treatments including active exercise therapy pre- and post-surgery. Conservative treatment without the addition of surgery is also a common treatment option, with appropriate exercise prescribed to strengthen the surrounding musculature of the shoulder, improve range of motion, and increase functional strength. As exercise therapy is used in conjunction with surgical interventions it is extremely difficult to determine if outcomes from either one is greater. Therapists are tending to lean more towards prescribing exercise therapy initially, as in a worst-case scenario this will still be great prehab for any potential surgical intervention in the future.
Upper Arm & Elbow
Medial Epicondylitis (Golfer’s Elbow)
Medial Epicondylitis is characterised as an overuse injury rather than an impact condition. Continuous movement (specifically gripping and rotation) of the forearm can cause microscopic tears in the tissue leading to inflammation and pain. Although it has earned its colloquial title from the sport this injury is not limited to Golfer’s, In fact 95% of individuals who are diagnosed with medial epicondylitis haven’t ever picked up a club.
Symptoms of Medial Epicondylitis include:
- Pain or swelling on the inside of elbow and wrist
- Pain when grasping or gripping objects
- Stiffness/soreness when straightening your arm
- Pain when rotating the forearm or wrist
Symptoms can be acute or have a delayed onset and range from mild discomfort to pain and avoidance of function if not treated correctly.
Golfer’s Elbow Treatment
Practical treatments of medial epicondylitis include range of motion and strengthening protocols for the wrist and forearm extensors (particularly for the extensor carpi radialis brevis). Current research indicates that progressive, incremental strengthening regimes are an effective treatment tool for increasing pain free function and mitigating the progression of the condition.
Individuals who engage in active rehabilitation early are often able to return to function with minimal discomfort within two weeks. If the condition is not conservatively managed early, alternative treatment modalities can be used with severe cases such as steroidal injections, autologous blood injections and surgery.
Lateral Epicondylalgia (Tennis Elbow)
Lateral Epicondylalgia is characterised as an overuse injury rather than an impact condition. Continuous movement (specifically gripping and rotation) of the forearm can cause microscopic tears in the tissue leading to inflammation and pain. It can also occur due to a current increase in load, or use of your forearm above and beyond your normal amount of activity. Although it has earned its colloquial title from the sport this injury is not limited to tennis players. In fact, more than 95% of individuals who are diagnosed with lateral epicondylalgia haven’t ever picked up a racket.
Symptoms of Lateral Epicondylalgia include:
– Pain or swelling on the outside of the elbow and wrist
– Pain when grasping or gripping objects
– Stiffness/soreness when straightening and bending your arm
– Pain when rotating the forearm or wrist, such as opening jars and doors
Symptoms can be acute or have a delayed onset and range from mild discomfort to severe pain and avoidance of function if not treated correctly.
Tennis Elbow Treatment
Practical treatments of lateral epicondylalgia include range of motion and strengthening protocols for the wrist and forearm extensors (particularly for the extensor carpi radialis brevis). Current research indicates that progressive, incremental strengthening regimes are an effective treatment tool for increasing pain free function and mitigating the progression of the condition.
Individuals who engage in active rehabilitation early are often able to return to function with minimal discomfort within two weeks. However, it is worth noting that pain may persist for some time afterwards. If the condition is not conservatively managed early, alternative treatment modalities can be used with severe cases such as steroidal injections, autologous blood injections and surgery but current research states this should be avoided for at least 12 weeks.
Forearm & Wrist
Repetitive strain injury (RSI)
RSI can present with or without associated swelling and can be difficult to diagnose. Other conditions may be present and contribute to the negative symptoms of RSI, Pathologies such as carpal tunnel or tendinopathy, although sometimes pain does presents without any tissue damage.
Improvement of RSI symptoms can occur quickly by making small adjustments to your routine. Trying to identify the activities that trigger your symptoms and reducing or eliminating this activity for a short period of time to rest the affected limbs can be helpful – although often this may not be possible. If ceasing the triggering activity is not an option, taking short breaks, often can be an option. Or potentially changing your set up, or changing up what you do often, so you aren’t doing the same thing for long periods of time.
Seeing an allied health professional such as an exercise physiologist or physiotherapist for long term management could be beneficial. Implementing exercise to strengthen and stretch the affected muscles has been shown to reduce negative symptoms and/or avoid a relapse.
Upper & Lower Back
Upper Cross Syndrome
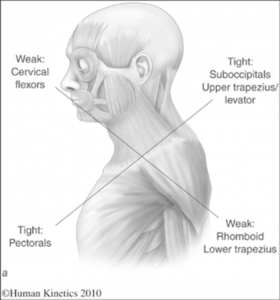
The postural change of a forward head position creates tightness of the upper trapezius and levator scapula, crossed with tightness of your pectoralis (chest) muscles. Deep neck flexors, as well as middle and lower trapezius muscles become weak. This imbalance can create joint dysfunction and pain. Postural changes include a forwards head posture, increased cervical lordosis, thoracic kyphosis, elevated and forwards rounded shoulders and winging of scapulae. This creates strain on both bony and muscular structures and can decrease shoulder joint stability.
Exercises, education on posture and manual therapy are the three combined and recommended components to manage this syndrome. Your Exercise Physiologist will be able to provide you with education on how to better manage your postures and pain. Working together, you and your Exercise Physiologist can identify any root causes to these postures and implement strategies to better manage these for long term success. You will be prescribed specific exercises to stretch tight and short muscles, as well as exercises to strengthen weak muscles. This educational and exercise therapy approach is best practice when it comes to managing and reversing Upper Cross Syndrome.
Thoracic Outlet Syndrome
Thoracic Radiculopathy
Non Specific Lower Back Pain
It is usually categorised as acute, sub-acute or chronic. Acute is characterised by pain less than 6 weeks, sub-acute is 6-12 weeks and chronic is when pain is present for 12 or more weeks.
Physical therapy is effective at treating and reducing NSLBP and is encouraged as a line of management for this condition. Periods of inactivity have been shown to exacerbate symptoms of NSLBP, highlighting the importance of exercise as part of your pain management. Our exercise therapists can assist you in education around NSLBP, pain pathways, and management techniques, as well as provide you a comprehensive exercise program to manage your pain.
Hip
Greater Trochanteric Pain Syndrome
Aetiology is multi-factorial involving both intrinsic and extrinsic factors. Some of the main factors are repetitive activity, mechanical overload, sedentary behaviours, obesity, and training error. Weaknesses around the hip muscles, particularly those of the hip abductors like gluteus medius, can cause increased valgus (knees angling in towards the midline of the body) and therefore increased strain on the gluteus medius and gluteus minimums tendons at the greater trochanter area. With this increase in angle of this femur, the iliotibial band compounds the strain on the gluteal tendons by compressive forces. This explains why pain in the sitting and prolonged sitting position causes pain since compression on these tendons is increased in this position. Exercise management should involve gradual loading of the tendons to recondition them to tolerate load. It is recommended that exercise should start at a low-moderate effort level with low repetitions. Resistance exercises should focus on building strength in the gluteal muscles but also the core muscles and other lumbopelvic stabilising muscles. Exercise management aims to strengthen the gluteal muscles and manage load around the hip joint to reduce pain and restore function.
Upper Leg
Quadriceps Muscle Strain / Tear
Physical therapy plays an important role in all stages post injury. Our Physiotherapist is able to provide manual techniques, education and exercises to support you through your rehabilitation and prevention of reinjury.
Knee
ACL Tear/Rupture
Although the occurrence of ACL injuries is vast, this often-devastating injury is largely preventable with muscular and neuromuscular exercise training.
ACL Injury Treatment
Once the injury is established, the first (and often only) treatment strategy considered is surgical ACL repair. This involves repair of reconstructing the ACL with a graft to provide stability for the knee. With the incidence of surgical reconstructions and revisions (Secondary ACL surgeries) in Australia being amongst the highest in the world and lead studies finding no significant difference in reported outcomes between surgery and conservative (Exercise) treatment, it is high time for considering exercise as the first treatment strategy. This treatment involves gradual progression through evidence-based flexibility, balance and strength exercises with an objective of returning to pre-injury function. This has been shown to not only successfully provide stability for the knee, but also allow reconnection of ACL tissue in some cases. It has also been repeatedly proven to improve surgical outcomes. Therefore, if function is not achieved with conservative treatment it has increased your chances for success with surgical treatment, making for perfect pre-operative preparation and minimising recovery times.
Patellofemoral Pain Syndrome (Runner’s Knee)
Patellofemoral Pain Syndrome is characterised as an overuse injury rather than an impact condition. Normal daily tasks such as running, walking, climbing up and down stairs / hills, as well as squatting become painful with Patellofemoral Pain Syndrome. It typically occurs after a sudden increase in load, or use of your legs above and beyond your normal amount of activity. Although it has earned its colloquial title from the sport this injury is not limited to runners and can occur even with a sudden increase in walking or gym activities.
The pain develops typically due to an imbalance between the muscles of the hips and thighs which move the knee and kneecap, resulting in a shift in the direction the kneecap moves during bending and straightening of the knee. Usually your kneecap slides in a groove created between your thigh and shin bone at the knee joint with no issues. When it is “grumpy” due to a sudden change in your physical activity levels, the kneecap no longer slides smoothly causing pain and discomfort.
Symptoms of Lateral Epicondylalgia include:
– Pain or swelling about your kneecap which can extend to the sides or even back of your knee
– Pain when squatting, walking, running, jumping, navigating stairs and hills
– Stiffness/soreness when straightening and bending your knee
– Pain and/or stiffness/tightness in your thighs and hips
Symptoms usually occur only with the above movements, typically disappearing as quickly as they start. They can be acute or have a delayed onset and range from mild discomfort to severe pain and avoidance of function if not treated correctly.
Patellofemoral Pain Treatment
Practical treatments of Patellofemoral Pain Syndrome include range of motion, flexibility and strengthening protocols for the surrounding muscles, including the gluteals, hamstrings, quadriceps and calves. Current research indicates that progressive, incremental strengthening regimes are an effective treatment tool for increasing pain free function and mitigating the progression of the condition.
Individuals who engage in active rehabilitation early are often able to return to function with minimal discomfort within 1-2 months. However, it is worth noting that pain may persist for some time afterwards. The current consensus for the best treatment method is a combination of exercise therapy, manual therapy, taping and foot orthotics. Surgery will not fix this condition. The general time taken to get better ranges from 2 weeks to 3-4 months depending on the case.
Lower Leg
Calf Muscle Strain
Physical therapy plays an important role in all stages post injury. Our Physiotherapist is able to provide manual techniques, education and exercises to support you through your rehabilitation and prevention of reinjury.
Ankle & Foot
Achilles Tendinopathy
Achilles Tendinopathy occurs when there has been a spike in the amount of exercise or physical activity you are doing. This tends to occur after a layoff and sudden return to exercise, such as in middle-aged people, or in physically active people who have suddenly upped the ante in their exercise routine. It occurs in sports/exercise with repetitive jumping or running, overusing the tissues leading to inflammation and pain.
It can also occur due to:
- Change in training surface
- Lack of training variation
- Incorrect footwear
- Excessive intensity or distance increase
Symptoms of Achilles Tendinopathy include:
– Pain or swelling on the bottom portion of your Achilles into your heel
– Pain with walking, running, jumping or steps
– Stiffness/soreness when straightening and bending your ankle
– Pain worse at night and/or first thing in the morning
Symptoms can be acute or have a delayed onset, ranging from mild discomfort to severe pain and avoidance of function, lasting for years if not treated correctly.
Achilles Tendinopathy Treatment
Practical treatments of Achilles Tendinopathy include range of motion and strengthening protocols for the ankle, calf and leg muscles. Current research indicates that progressive, incremental strengthening regimes are an effective treatment tool for increasing pain free function, enabling a return to your job, sport or recreation activities.
You should be able to make a return to these within 2-4 weeks depending on the severity. You will then be able to perform at your fullest with time over the next few months or so. However, your pain may continue for a while then though you are able to function at a much higher level than before.
The addition of manual therapy has also shown to assist with pain relief to help you return to the painful tasks quicker.
If the condition is not conservatively managed early, alternative treatment modalities can be used with severe cases such as steroidal injections and autologous blood injections but current research states this should be avoided for at least 12 weeks.
Ankle Sprain
Ankle injuries are often considered trivial injuries which will get better without any effort, but this is not the case. Australian research has shown around one third of ankle sprains become chronic up to seven years after the injury.
Common causes of a Rolled Ankle include:
- Playing sports that involve jumping, running, twisting, changing of direction or pivoting movements
- Uneven surfaces
- Wearing inappropriate footwear for the task
- Previous ankle injuries
- Poor physical condition such as poor overall fitness, being overweight, and reduced ankle strength and flexibility
Symptoms of a Rolled Ankle include:
- Pain with placing your weight onto the ankle and with walking
- Tenderness to touch
- Ankle stiffness
- Bruising
- A popping or cracking sound at the time of injury
- Poor balance and feeling instability about the ankle
There are three types of Rolled Ankles:
- Grade I: only a few ligament fibres are torn – often return to sport within 2-4 weeks
- Grade II: less than 50% of ligament fibres are torn – often return to sport within 8 weeks
- Grade III: a complete tear of the ligament – often return to sport about 12 weeks
Ankle Sprain Treatment
Rolled Ankle injury treatment is split between acute and later stages management.
Acute management involves following the acronym PEACE. This stands for Protect, Elevate, Avoid Anti-Inflammatories, Compression and Ice, and Education (from the health professional). Basically, avoid activities that worsen your pain, do the activities that you can and rest from ones you can’t, and then elevate, compress and ice the ankle when resting. Pain medication may help too.
After a few days of the above, you can then give your ankle LOVE. This stands for Load, Optimism, Vascularisation and Exercise. Basically, resume normal activities as much as possible based off of your symptoms, maintain a positive outlook and begin a strengthening, mobility and balance exercise program under the supervision of a health professional.
Doing the above should ensure you do not have ongoing issues in the years to come. In fact, engaging in the above often results in people returning to normal activities within a couple of weeks (if it is a grade I injury).
Plantar Fasciopathy
Plantar fasciopathy is common in both active and less active people. It often arises due to a sudden increase in load or activity beyond what is your normal amount.
Other risk factors for Plantar Fasciopathy include:
- Calf muscles tightness
- Calf muscles weakness
- Low arches, flat feet or high arches
- Being overweight
- Wearing shoes with poor arch support for sustained periods
- Being on your feet for extended periods of time on hard surfaces
Symptoms of Plantar Fasciopathy include:
- Pain in the heel or arch region
- Pain in the morning with your first few steps which often eases with more steps
- Pain with walking after being still for a while
- Pain with standing for extended periods of time
- Tightness in the calf muscles
Symptoms can be acute or have a delayed onset, ranging from mild discomfort to severe pain and avoidance of function if not treated correctly.
Plantar Fasciopathy Treatment
Practical treatments of plantar fasciopathy include range of motion and strengthening protocols for the foot, ankle, calf and knee. Current research indicates that progressive, incremental strengthening regimes are an effective treatment tool for increasing pain free function and preventing the progression of the condition.
Individuals who engage in active rehabilitation early are often able to return to function with reduced pain and discomfort within two weeks. A combination of manual therapy and exercise rehabilitation can often provide superior improvement in pain and function. However, it is worth noting that pain may persist for some time afterwards even though you are able to do more.
Other options include simple pain relief such as paracetamol, taping techniques and inserts to reduce the pressure on your heel and plantar fascia.
Other management strategies such as injections and surgery should be avoided where possible as they do not provide extra improvements long term.