Occupational Health
Neck pain
Occupational neck pain, forward head posture, text neck, there are many names that are thrown about when referring to non-specific neck pain. Neck pain is commonly reported among office workers, or those who spend long periods of time sitting such as students. Posture is often blamed for neck and back pain; however multiple studies show that there is little to no correlation between the two. Rather, loss of range of motion (ROM), low muscle strength & inactivity have a stronger correlation with neck pain. Weakness of the muscles in the neck, back, and shoulders may be evident in those presenting with non-specific neck pain. Exercise and manual therapy, or a combination of the two have been shown to be the best course of treatment. Individualised assessment and prescription designed to strengthen and improve ROM can drastically improve pain levels. Other passive therapies such as heat, acupressure, trigger point and stretching may provide acute relief and could also be helpful when used in conjunction with a manual therapy and exercise.
Postural Kyphosis
Kyphosis is defined by an excessive curvature of the thoracic spine which is characterised by forward rounding of the upper back and shoulders. It can arise from genetics, age and poor postures. Kyphosis into adulthood and the elderly population can be associated with significant health impairments. In severe cases it has been linked to underlying conditions such as osteoporosis, vertebral fractures, degenerative disk disease and spinal extensor muscle weakness. Exercise and physical therapy can have benefits for each type of Kyphosis. Due to the nature of Kyphosis and the accompanied increase in risk of underlying conditions, exercise and interventions need to be tailored accordingly. Specific and tailored exercises can aim to relieve pain and improve postures. Exercise therapy not only provides physiological benefits for those with Kyphosis, but it has also been shown to improve self-image, confidence and self-satisfaction with appearance.
Postural kyphosis is the most common type and arises from poor postures. It can occur in any age group from childhood, during rapid growth phases, adulthood, and elderly population. It commonly presents itself in adolescence and elderly population and is clinically noted as poor posture. Poor postures and forward slouched postures create stress and stain on ligaments and muscles that support the spine. Prolonged strain and cause these muscles to become weak and long and muscles through the front of the upper body to become short. Postural Kyphosis is not typically associated with severe structural abnormalities of the spine itself and can be corrected when sitting up straight. However, prolonged poor postures and curvature in the spine can increase risk of underlying bone and muscle conditions. Strengthening of the muscles supporting the spine and abdomen as well as posture training have been shown to reduce clinical measures of Postural Kyphosis
Postural kyphosis is the most common type and arises from poor postures. It can occur in any age group from childhood, during rapid growth phases, adulthood, and elderly population. It commonly presents itself in adolescence and elderly population and is clinically noted as poor posture. Poor postures and forward slouched postures create stress and stain on ligaments and muscles that support the spine. Prolonged strain and cause these muscles to become weak and long and muscles through the front of the upper body to become short. Postural Kyphosis is not typically associated with severe structural abnormalities of the spine itself and can be corrected when sitting up straight. However, prolonged poor postures and curvature in the spine can increase risk of underlying bone and muscle conditions. Strengthening of the muscles supporting the spine and abdomen as well as posture training have been shown to reduce clinical measures of Postural Kyphosis
Upper Cross Syndrome
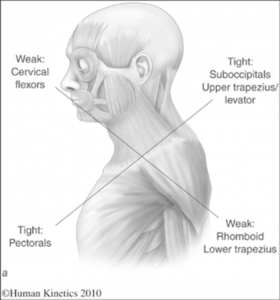
Upper Cross Syndrome is directly caused by continual poor postures such as prolonged sitting with a forward head position. These prolonged positions cause muscles in the neck, shoulders and chest to negatively adapt in order to compensate for this persistent strain. This posture causes muscles of the posterior chain (back of your body) to become strained and overactive and muscles of your anterior chain (front of your body) to become tight and short. The combination of overactive and underactive muscles crosses over causing an X-Shape to develop, the image below.
The postural change of a forward head position creates tightness of the upper trapezius and levator scapula, crossed with tightness of your pectoralis (chest) muscles. Deep neck flexors, as well as middle and lower trapezius muscles become weak. This imbalance can create joint dysfunction and pain. Postural changes include a forwards head posture, increased cervical lordosis, thoracic kyphosis, elevated and forwards rounded shoulders and winging of scapulae. This creates strain on both bony and muscular structures and can decrease shoulder joint stability.
Exercises, education on posture and manual therapy are the three combined and recommended components to manage this syndrome. Your Exercise Physiologist will be able to provide you with education on how to better manage your postures and pain. Working together, you and your Exercise Physiologist can identify any root causes to these postures and implement strategies to better manage these for long term success. You will be prescribed specific exercises to stretch tight and short muscles, as well as exercises to strengthen weak muscles. This educational and exercise therapy approach is best practice when it comes to managing and reversing Upper Cross Syndrome.
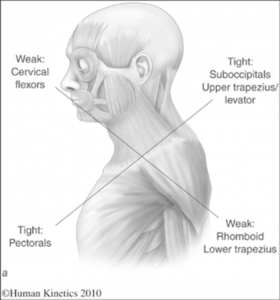
The postural change of a forward head position creates tightness of the upper trapezius and levator scapula, crossed with tightness of your pectoralis (chest) muscles. Deep neck flexors, as well as middle and lower trapezius muscles become weak. This imbalance can create joint dysfunction and pain. Postural changes include a forwards head posture, increased cervical lordosis, thoracic kyphosis, elevated and forwards rounded shoulders and winging of scapulae. This creates strain on both bony and muscular structures and can decrease shoulder joint stability.
Exercises, education on posture and manual therapy are the three combined and recommended components to manage this syndrome. Your Exercise Physiologist will be able to provide you with education on how to better manage your postures and pain. Working together, you and your Exercise Physiologist can identify any root causes to these postures and implement strategies to better manage these for long term success. You will be prescribed specific exercises to stretch tight and short muscles, as well as exercises to strengthen weak muscles. This educational and exercise therapy approach is best practice when it comes to managing and reversing Upper Cross Syndrome.
Repetitive strain injury (RSI)
RSI is an umbrella term used to describe pain felt in soft tissue usually in the upper limbs caused by repetitive movement and overuse. There are a few main symptoms associated with RSI this includes nerve type pain (burning, aching, shooting pain), tremors, numbness, lack of strength or fatigue. RSI can flare up during activities of daily living such as turning on taps, opening doors, using a computer mouse, chopping vegetables and can be quite debilitating for those that experience it.
RSI can present with or without associated swelling and can be difficult to diagnose. Other conditions may be present and contribute to the negative symptoms of RSI, Pathologies such as carpal tunnel or tendinopathy, although sometimes pain does presents without any tissue damage.
Improvement of RSI symptoms can occur quickly by making small adjustments to your routine. Trying to identify the activities that trigger your symptoms and reducing or eliminating this activity for a short period of time to rest the affected limbs can be helpful – although often this may not be possible. If ceasing the triggering activity is not an option, taking short breaks, often can be an option. Or potentially changing your set up, or changing up what you do often, so you aren’t doing the same thing for long periods of time.
Seeing an allied health professional such as an exercise physiologist or physiotherapist for long term management could be beneficial. Implementing exercise to strengthen and stretch the affected muscles has been shown to reduce negative symptoms and/or avoid a relapse.
RSI can present with or without associated swelling and can be difficult to diagnose. Other conditions may be present and contribute to the negative symptoms of RSI, Pathologies such as carpal tunnel or tendinopathy, although sometimes pain does presents without any tissue damage.
Improvement of RSI symptoms can occur quickly by making small adjustments to your routine. Trying to identify the activities that trigger your symptoms and reducing or eliminating this activity for a short period of time to rest the affected limbs can be helpful – although often this may not be possible. If ceasing the triggering activity is not an option, taking short breaks, often can be an option. Or potentially changing your set up, or changing up what you do often, so you aren’t doing the same thing for long periods of time.
Seeing an allied health professional such as an exercise physiologist or physiotherapist for long term management could be beneficial. Implementing exercise to strengthen and stretch the affected muscles has been shown to reduce negative symptoms and/or avoid a relapse.
Non-Specific Lower Back Pain
Nonspecific lower back pain (NSLBP) is lower back pain that is not attributable to a known pathology such as fracture, disc pathology, osteoporosis, and radicular syndrome among other pathologies. Lower backpain is common in our modern society with 60-80% of people reporting pain throughout their lifetime, causing more global disability than any other condition.
It is usually categorised as acute, sub-acute or chronic. Acute is characterised by pain less than 6 weeks, sub-acute is 6-12 weeks and chronic is when pain is present for 12 or more weeks.
Work place stressors or inactivity in the workplace (e.g. desk work / being stationary) can be factors contributing to lower back pain. Physical therapy is effective at treating and reducing NSLBP and is encouraged as a line of management for this condition. Periods of inactivity have been shown to exacerbate symptoms of NSLBP, highlighting the importance of exercise as part of your pain management. Our exercise therapists can assist you in education around NSLBP, pain pathways, and management techniques, as well as provide you a comprehensive exercise program to manage your pain.
It is usually categorised as acute, sub-acute or chronic. Acute is characterised by pain less than 6 weeks, sub-acute is 6-12 weeks and chronic is when pain is present for 12 or more weeks.
Work place stressors or inactivity in the workplace (e.g. desk work / being stationary) can be factors contributing to lower back pain. Physical therapy is effective at treating and reducing NSLBP and is encouraged as a line of management for this condition. Periods of inactivity have been shown to exacerbate symptoms of NSLBP, highlighting the importance of exercise as part of your pain management. Our exercise therapists can assist you in education around NSLBP, pain pathways, and management techniques, as well as provide you a comprehensive exercise program to manage your pain.